Curious to know what exactly the low fermentation diet is and how it differs from the low FODMAP diet? Read on to get the breakdown and find out if there is evidence to support it!
If you have been diagnosed with small intestinal bacterial overgrowth (SIBO), then I’m sure you’re scouring the internet for more information. One name that you’ll likely see referenced frequently is Dr. Mark Pimentel from Cedars-Sinai Hospital. He’s been at the forefront of uncovering what SIBO is and how it’s best treated. Dr. Pimentel and his team frequently use the low fermentation diet to help manage their patient’s digestive symptoms.
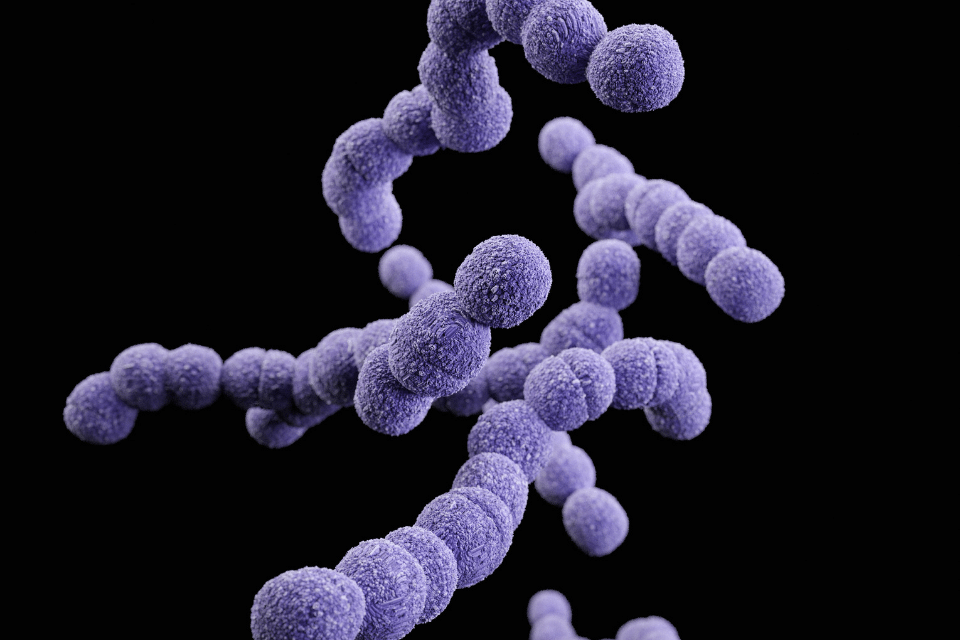
What is SIBO?
We’ve talked about SIBO in a previous blog post but as a quick refresher, it’s basically an overgrowth of bacteria in your small intestine. One myth is that the bacteria are “bad”, which is not exactly the case. Most of your gut bacteria should be in your large intestine (i.e. colon), but when you have SIBO, something causes the bacteria to overpopulate in the small intestine instead. There is no one specific cause of SIBO, but treatment is typically antibiotics to reduce the bacteria and some type of diet to help with symptom relief.
If you’ve completed a quick Google search for “SIBO Diet”, then I’m sure you’ve seen names like the specific carbohydrate diet (or SCD) diet, the GAPS diet, the SIBO specific (or biphasic) diet, the low FODMAP diet, and the low fermentation (or Cedars Sinai diet). While I could write many blog posts on the pros and cons of each diet, today we’re only going to focus on the low fermentation diet and how it differs from the low FODMAP diet.
The Low Fermentation Diet
The low fermentation diet is actually very similar to the low FODMAP diet and oftentimes less restrictive! It focuses on a reduction in high fiber foods (like whole-wheat bread) while promoting the consumption of easy-to-digest carbohydrates (like white bread, rice, or potatoes). The diet also focuses on the importance of meal structure and timing. This is due to the Migrating Motor Complex (MMC). The MMC is like a cleaning wave that occurs every 90-120 minutes in your small intestine. This cleaning wave helps move all the leftover debris from your food, along with microbes, out of the way and into the colon. For this to occur, you need to be in a fasting state. When SIBO occurs, the bacteria that are in the small intestine (aka the wrong place) start feeding on any food that makes it through there. If you are practicing meal spacing during treatment, this ensures that bacteria won’t have as much to munch on and thus can’t cause as many symptoms.
So, what exactly can you eat on the low fermentation diet? A lot, actually! Like I previously mentioned, easy-to-digest or simple carbohydrates are perfectly fine. Proteins and fats are ok too. The diet endorses “anything that grows from the ground” like potatoes, carrots, beets, carrots, onion, and garlic. Yes, onion and garlic. If you’re familiar with the Low FODMAP diet, you know that those are two big things that are off-limits! Things to avoid include all legumes, cruciferous vegetables (like broccoli and brussels sprouts), and certain fruits like bananas, apples, and pears. Yogurt is also off-limits, but lactose-free milk and hard cheeses are ok. The diet also allows for “cheats” like lactose-free ice cream and encourages you NOT to stress yourself out when eating out.
The Difference between low FODMAP and low fermentation
There are actually a lot of differences. Many foods that are allowed on the low fermentation diet are off-limits for low FODMAP or at least have a small portion size. I think the biggest difference is the allowance of garlic and onion on low fermentation, but not low FODMAP. Beans and legumes vary on the low FODMAP diet, but it really comes down to how they’re prepared and the portion size that you’re eating. Here’s a short review of some key differences:
- Vegetables
- Low FODMAP: Starchy veggies like rice and potatoes are fine, but things like asparagus, beets, broccoli, and celery have a small serving size. Cauliflower, button mushrooms, garlic, and onion are all considered high FODMAP.
- Low Fermentation: Most seem to be allowed, including mushrooms, garlic, and onions. Cruciferous vegetables like broccoli, cabbage, brussels sprouts, cauliflower, and leafy vegetables are to be avoided (even in small amounts).
- Fruits
- Low FODMAP: Fruits vary based on what FODMAP group they fall into (sorbitol, mannitol, fructan, etc). Things like apples, pears, blackberries, and watermelon are considered high FODMAP.
- Low Fermentation: All fruits are fine, but it’s recommended that apples, pears, and bananas are limited because they’re constipating (Take that with a grain of salt!).
- Beans/Legumes
- Low FODMAP: Canned beans are typically lower in FODMAP content, but some dry beans are allowed. It really comes down to the portion size. Things like chickpeas have a pretty good portion size, while black beans and kidney beans are much smaller servings.
- Low Fermentation: Beans and legumes are completely off-limits.
- Nuts and seeds
- Low FODMAP: Cashews and pistachios are off-limits, but most seeds and nuts are fine with reasonable portion size.
- Low Fermentation: All nuts are fine, no mention of seeds.
- Grains
- Low FODMAP: Whole grains like rice, quinoa, and oats are allowed, in addition to small amounts of wheat pasta or bread (i.e. white). Sourdough bread is also allowed.
- Low Fermentation: Products made from white flour are fine. The diet mentions that the gluten-free diet is also fine because it’s a low carbohydrate diet (this is false). Gluten is a protein and therefore has nothing to do with either diet.
The Evidence
- There have been no clinical trials on either the low fermentation diet or the low FODMAP diet for SIBO.
- We know that a low FODMAP diet is an effective tool for managing IBS symptoms. However, we don’t have any evidence that it does the same for SIBO. The reason that it is used in symptom management of SIBO is due to the reduction in fermentable carbohydrates.
- The Low Fermentation diet may be less restrictive in terms of what you can eat, but some people may struggle with the timing/lack of grazing.
The Bottom Line
Neither the low FODMAP nor low fermentation diet is meant to be followed long term. We know that long-term restrictions may negatively impact the microbiome as well as put people at risk for disordered eating. These diets are also not meant to eradicate SIBO (that requires antibiotics or antimicrobials). At this point, diet is mainly used to help with symptom management. If you experienced any deficiencies as a result of SIBO (i.e. vitamin D or B12), then your diet will likely focus on replenishing those nutrients as well. Hopefully, we’ll have studies in the future that give us more definitive guidance. Until then, I recommend working with your healthcare provider or dietitian to come up with the diet that makes the most sense for you while also giving you symptom relief.
References
Bolte L.A., Vich Vila A., Imhann F., et al. “Long-term dietary patterns are associated with pro-inflammatory and anti-inflammatory features of the gut microbiome” Gut 2021; 70:1287-1298.
“Cedars-Sinai Expert Shares the Latest Medical Insights to Help Patients with IBS.” cedars-sinai.org. Cedars-Sinai, April 19, 2021. https://www.cedars-sinai.org/newsroom/irritable-bowel-syndrome-mark-pimentel-md/